Peri-Implantitis

What Is Peri-Implantitis?
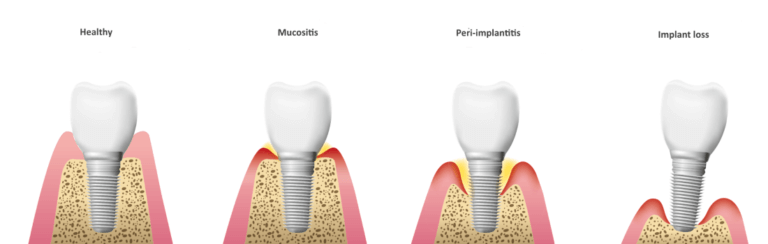
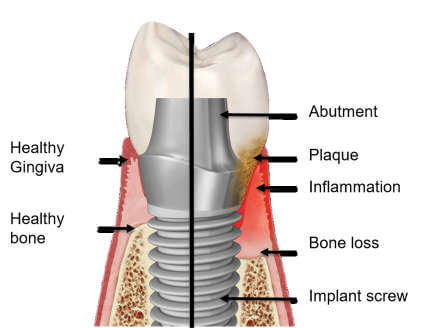
Peri-implantitis is a type of gum disease that affects the tissue and bone surrounding dental implants. It is caused by the buildup of bacteria and plaque around the implant site, leading to inflammation and infection. Left untreated, peri-implantitis can result in discomfort, gum and bone loss, and even the failure of the dental implant.
Before you contact a Toronto dentist to examine possible Peri-Implantitis, there are some things you should know as a patient:
- Why Do I Have Peri-Implantitis?
- Signs And Symptoms Of Peri-Implantitis
- Treatment Options For Peri-Implantitis
- Managing Peri-Implantitis Until You Can See The Dentist
- Frequently Asked Questions About Peri-Implantitis
If you have questions about Peri-Implantitis or other dental problems, please contact us for more information
Why Do I Have Peri-Implantitis?
Peri-implantitis can develop due to several factors, including:
- Poor Oral Hygiene: Failing to properly clean around the implant can lead to plaque buildup, which increases the risk of infection.
- Smoking: Tobacco use compromises healing and the body’s ability to fight infections, making peri-implantitis more likely.
- Medical Conditions: Conditions like diabetes or a weakened immune system can hinder your body’s ability to heal and fight off infections.
- Improper Implant Placement: Misaligned implants or poorly fitted restorations can create areas where bacteria thrive.
- Genetic Predisposition: A family history of gum disease or previous gum issues may increase your risk.
- Poorly Fitted Restorations: Ill-fitting crowns or bridges can trap bacteria, leading to inflammation around the implant.
Identifying the cause of your peri-implantitis is crucial for determining the best course of treatment. If you have further questions about Peri-Implantitis, please contact us.
Signs And Symptoms Of Peri-Implantitis
It’s essential to recognize the symptoms early to prevent serious complications. Common signs of peri-implantitis include:
- Bleeding Gums: Bleeding around the implant when brushing or flossing.
- Red, Swollen Gums: Inflammation and redness around the implant site.
- Pain or Discomfort: Persistent tenderness near the implant.
- Implant Loosening: A wobbly or unstable implant is a sign of bone loss.
- Pus or Discharge: Yellow or green discharge, along with a foul taste, may indicate infection.
If you notice any of these symptoms, consult your dentist immediately for diagnosis and treatment. If you have further questions about signs and symptoms of Peri-Implantitis, please contact us.
Treatment Options For Peri-Implantitis
Treating peri-implantitis involves controlling the infection, stopping the progression of the condition, and restoring oral health. Treatment options include:
- Professional Cleaning: Deep cleaning removes plaque and bacteria from around the implant.
- Antibiotics: Prescription antibiotics may be used to reduce infection and inflammation.
- Debridement Surgery: Advanced cases may require surgical removal of infected tissue to promote healing.
- Implant Removal: In severe cases with significant bone loss, the implant may need to be removed. A bone graft can prepare the area for a new implant later.
Prompt treatment improves the chances of saving the implant and protecting surrounding tissues. If you have further questions about your treatment options for Peri-Implantitis, please contact us.
Managing Peri-Implantitis Until You Can See The Dentist
If you suspect peri-implantitis but cannot see your dentist right away, these measures can help:
- Rinse with Salt Water or Antiseptic Mouthwash: This reduces bacteria and soothes inflamed tissues.
- Use a Soft-Bristled Brush: Gently clean the area without irritating the gums.
- Avoid Smoking: Smoking worsens inflammation and slows healing.
- Take Over-the-Counter Pain Relievers: Medications like ibuprofen can reduce discomfort and swelling.
- Avoid Hard Foods: Stick to soft foods to minimize pressure on the implant.
These steps are temporary solutions and should not replace professional treatment. If you have further questions about Peri-Implantitis, please contact us.
Frequently Asked Questions About Peri-Implantitis
- Can peri-implantitis be reversed?
Yes, in its early stages, peri-implantitis can often be reversed with professional teeth cleaning and improved oral hygiene. Advanced cases may require surgical intervention.
- How common is peri-implantitis?
Studies suggest that peri-implantitis affects 10–20% of dental implant patients. The risk increases with poor hygiene or pre-existing gum disease.
- Is peri-implantitis painful?
In its early stages, peri-implantitis may not cause pain. However, as it progresses, you may experience tenderness, swelling, or discomfort.
- How can I tell the difference between normal healing and peri-implantitis?
Some swelling and discomfort are normal after implant placement. If symptoms persist, worsen, or include bleeding, pus, or implant looseness, consult your dentist.
By understanding peri-implantitis and taking proactive measures, you can protect your implants and maintain excellent oral health. Contact us today if you suspect peri-implantitis or have any questions about your dental implants!